|
Getting your Trinity Audio player ready...
|

Head and neck cancer continues to rank among the six most prevalent cancers globally, claiming hundreds of thousands of lives each year. Now, a sweeping new review is spotlighting a critical but underexplored factor in the disease’s progression: the interplay between energy metabolism and immune regulation.
Researchers say this dynamic relationship may be key to understanding why these cancers grow aggressively and resist treatment. The review, published this week in a leading oncology journal, outlines how tumor cells undergo extensive metabolic reprogramming—altering how they process glucose, lipids, and amino acids—to fuel growth and evade immune detection.
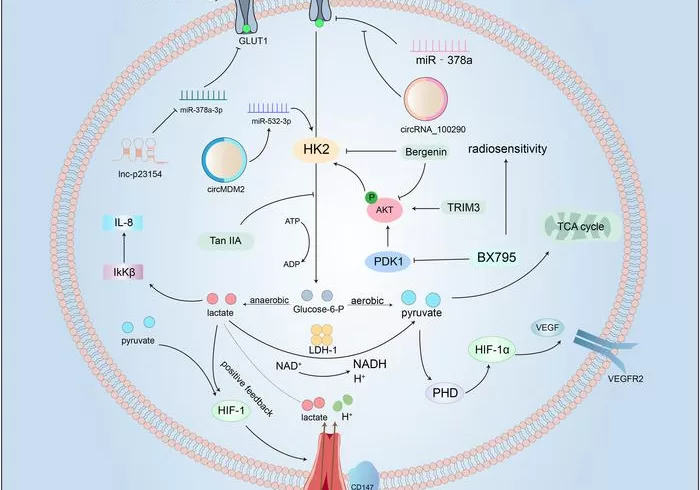
The study details how cancer cells accelerate glycolysis, the breakdown of glucose, which floods the tumor microenvironment with lactate. This not only supports rapid cell division but also suppresses immune responses.
Lipid metabolism is similarly hijacked, aiding in cell membrane production and energy storage while promoting immune evasion. Amino acid pathways, particularly those involving glutamine and arginine, are also restructured to support tumor expansion and manipulate immune cell behavior.
The immune system’s ability to fight cancer is significantly compromised. CD8⁺ T cells and other immune defenders are starved of nutrients, while immune checkpoints like PD-L1 are upregulated, effectively silencing immune attacks. Additional disruptions in antigen presentation and cytokine signaling further deepen the immunosuppressive environment.
Therapeutic Potential on the Horizon
Crucially, the review emphasizes that this metabolism–immunity axis is not merely a consequence of cancer—it’s a promising therapeutic target. Strategies such as blocking glucose transporters, disrupting lipid synthesis, and limiting amino acid availability could restore immune function. When combined with immunotherapy, these metabolic interventions may offer new hope for patients, especially those unresponsive to conventional treatments.
As researchers continue to unravel the biochemical crosstalk driving head and neck cancers, the findings could pave the way for more personalized and effective treatment approaches in the near future.