|
Getting your Trinity Audio player ready...
|
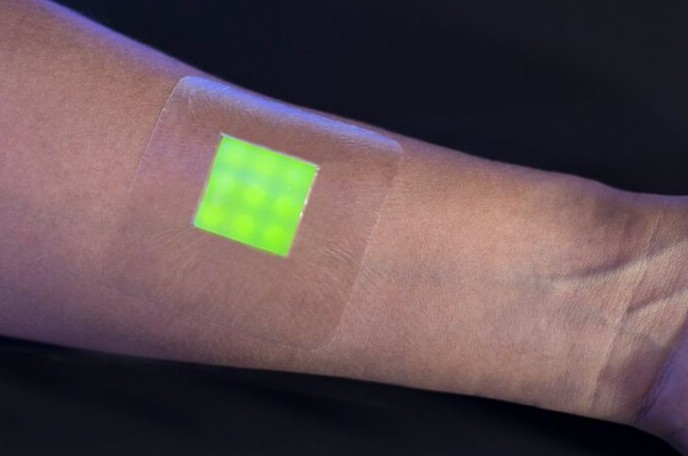
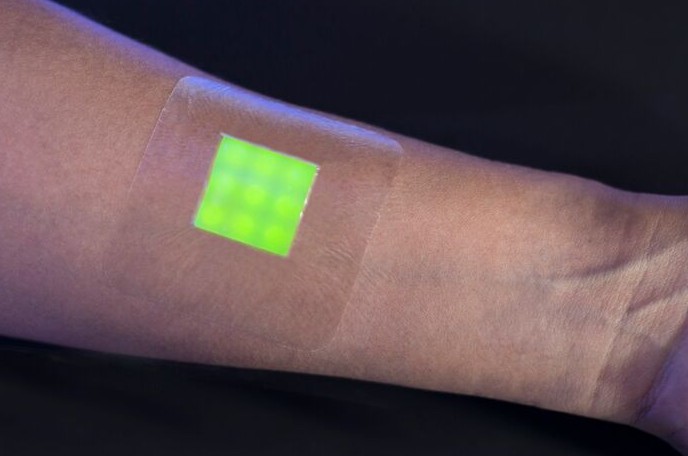
A new ‘smart’ wound dressing developed at the University of Bath in England could aid in the fight against antibiotic resistance by helping doctors to quickly determine if a burn patient’s wounds are infected, and prevent the unnecessary prescribing of antibiotics.
[pullquote]The ‘smart’ bandage works because of fluorescent dye-filled nanocapsules, which break open only when they come in contact with toxins produced by disease-causing bacteria in the wound.[/pullquote]
Wired reported that it currently takes up to 48 hours for doctors to determine if a burn patient’s wounds are actually infected, which leads to prescribing antibiotics as a precaution even if infection is not confirmed. Antibiotic resistance is a growing concern worldwide. The CDC reported that 50 percent of all antibiotics prescribed in U.S. health provider offices are either unnecessary, or inappropriate.
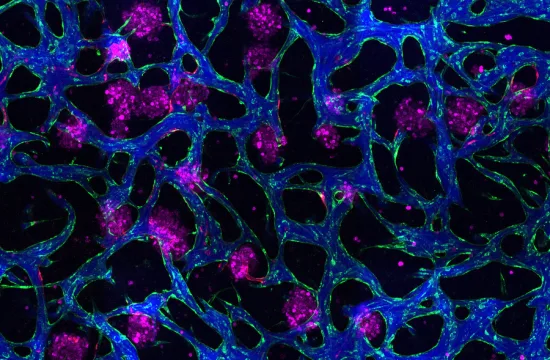
The ‘smart’ bandage works because of fluorescent dye-filled nanocapsules, which break open only when they come in contact with toxins produced by disease-causing bacteria in the wound, according to the Medical Research Council. Within hours doctors can see if the glow-in-the-dark dye appears on a patient, without having to remove bandages and subject patients to more pain and distress.
Dr. Toby Jones, who led the study, told Wired: “The nanocapsules mimic skin cells in that they only break open when toxic bacteria are present. They aren’t affected by the harmless bacteria that normally live on healthy skin.”
The Medical Research Council recently funded $1 million to researchers to test how accurate the dressing is at detecting infection in wound swabs and blister fluid from patients, as well as to develop a prototype for testing on patients.