MADISON — Some genetic mutations linked to leukemia are less than useful guides to making treatment decisions for patients. A new study from the University of Wisconsin–Madison suggests a group of clinical signs that can be paired with genetic testing to better inform the timing of more aggressive treatment.
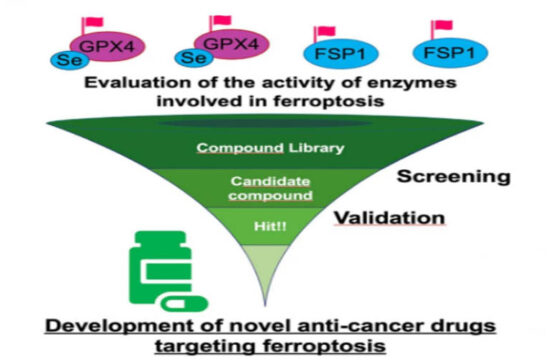
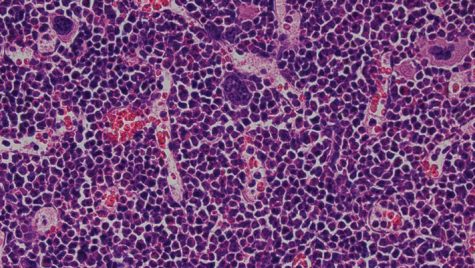
Studies of leukemia, which is cancer of the blood and blood-forming cells, have revealed alterations in genes that can be associated with the disease, and these genetic changes can be passed from one generation to the next. In certain cases, these alterations give doctors a way to gauge disease risk. For others, the consequences remain obscure. Even when the link between a particular genetic red flag and disease is strong, it may be difficult to pinpoint when serious stages of the disease may begin.
“That can be extremely variable. In a family that shares a common mutation, a grandfather might not present with symptoms until leukemia abruptly emerges,” says UW–Madison cancer researcher Alexandra Soukup. “By contrast, one of their grandchildren with the same genetic alteration may have serious symptoms starting at age seven — like lymphedema, which is severe swelling in the arms and legs, or low blood cell levels called cytopenia, which can cause life-threatening infections. We want to know what environmental and genetic factors trigger the disease presentation.”
Clinicians treating patients with genetic mutations likely to cause leukemia would like to know as well, because their options range from light-handed monitoring or drugs to invasive procedures including radiation, chemotherapy and stem cell transplants.
“Right now, the gold standard for treatment is a bone marrow transplant,” Soukup says. “But those occur when there’s already relatively severe disease presence, elderly patients are often not eligible for a transplant, and there can be life-threatening reactions to transplants.”
The complications of leukemia, which causes the bone marrow to make too few blood cells or abnormal blood cells, can be triggered by exposure to a pathogen or toxin, requiring the body to ramp up production of new blood cells.
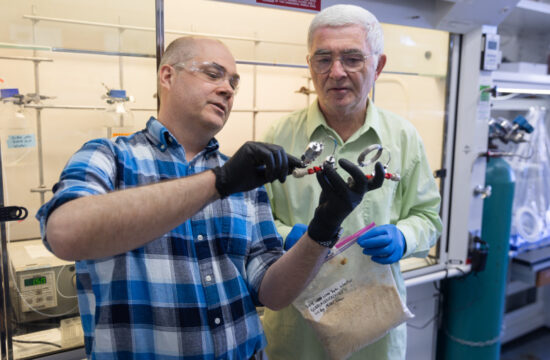
Soukup, a UW–Madison Cell & Regenerative Biology professor, and Emery Bresnick, director of the Wisconsin Blood Cancer Research Institute, and collaborators exposed mice harboring a genetic mutation associated with leukemia to “triggers” that created a model for bone marrow failure. This often precedes the development of leukemia. The researchers published their findings recently in the journal Science Advances.
“These mutations have little to no impact on the steady-state production of blood cells, and the mice containing the mutation might seem normal most of the time,” says Soukup, a scientist in Bresnick’s lab. “It’s just when you expose them to other stresses that severe defects emerge.”
The researchers stressed the mice in one of three ways, to mimic in a short time the sort of environmental and immunological challenges humans may face over longer terms — with a common chemotherapy drug, a component in bacterial cell walls that causes inflammation, or a drug used to ramp up stem cell division before human transplants. They wanted to see how the mice’s bone marrow would respond. In healthy marrow, stem cells should divide and mature into new blood cell producers to pick up the slack in times of trouble.
“In all of our cases, the stem cells seemed relatively normal, but they failed to respond or were extremely impaired in their response to expand,” Soukup says. “With the chemotherapeutic, you’d expect the stem cells to expand greatly and blood cells to regenerate, replacing what was destroyed by the chemotherapy. My mutant animals failed to mount a response.”
Without the stem cell expansion, the animals were overcome by bone marrow failure.
By exploring the ways in which the mutant mice responded to these stressors, the researchers can understand the sorts of human health issues — like recurring infections — that may bring on a life-threatening leukemia.
“Our mouse model provides a unique system to discover what may trigger severe disease presentations in humans, and we can use this system to develop strategies to counteract or nullify the triggering. We would want to apply such strategies to patients,” Soukup says. “If you’ve already presented with X, Y and Z, and you’ve been exposed to these risk factors, this may enable medical decisions to avoid the crisis scenario in which severe disease rapidly emerges.”
This research was supported by grants from the National Institutes of Healt and Scholar Awards to Dr. Soukup from the Leukemia & Lymphoma Society and American Society of Hematology.